
What inspired me to be a Mental Health Provider
I am known as Star to my clients, family and friends. I come from several decades of coms from an acute care background (ER,and various ICU specialities), Informatics, Research and Evidence Based Practice, Education and Community Health Nursing. I also love to write and share my views on health, wellness, and mental health.
After working with psychiatric patients in the Emergency Room, I realized that the healthcare system has done a huge disservice by its fragmented approach to treating clients in mental health. Getting sick during the pandemic and being privy to the ensuing post pandemic mental health crisis, I decided to further train as a Psychiatric Mental Health Nurse Practitioner (PMHNP).
Humans have the natural ability and resilience to heal themselves. As a PMHNP, my goal is to empower patients to gain back the confidence and belief that they are capable of recovering from life’s traumatic experiences. I am driven by how my colleagues and the community has been affected by the Pandemic. We as consumers of healthcare, have been led to believe that we are powerless against a healthcare system that doesn’t have the right infrastructure to support the magnitude and complexity of mental health issues.
Having to go through my own trauma of being sick with COVID, not being able to breathe and just being helpless for the first time, I came to understand the barriers that stand in the way of clients and the healthcare service that they deserve. Being in healthcare for many years, I never thought that I would be on the receiving end of services that really didn’t serve me well.
The Pandemic was the worst of times, and also the best of times. The skyrocketing numbers of mental health issues from various age groups post pandemic, is not only overwhelming the already exhausted healthcare delivery system and burnt out providers, but it also opened up several avenues on how we can be better prepared for what will continue to for decades.

What is mental health?
In a Rush: Does This Work for Mental Health
I would like to think of myself as a prudent mental health provider. Every week I try to keep up with the latest and best strategies to improve outcomes in mental health and behavioral clinics. Because I felt rushed, and unsuccessful with 30 minute intake appointments and 15 minute med management follow ups, I decided to terminate my recent contract with a high volume, for profit mental health clinic. I got paid $60.00 for a new patient, and $30.00 for follow up appointments. In order for me to actually afford to pay my student loans and eat, I have to see at least 2 intakes per hour or 4 (15min) follow up appointments every hour. Sans factoring in EHR issues, not having an MA to answer patients, PAs and pharmacy calls, processes flow issues etc. I was becoming the provider whom I didn’t want to be. I become almost robotic, straight to the point, and pressured. The office staff was constantly trying to text me to remind me that there are patients waiting impatiently to see me. Each time I try to walk my patient out the door, I was ready to walk out with them. Finally, I did.
I know LinkedIn include mid level providers, consumers of mental health care and advocacy leaders. Let me pose this question to all of you: What is your mental health care/wellness worth to you?
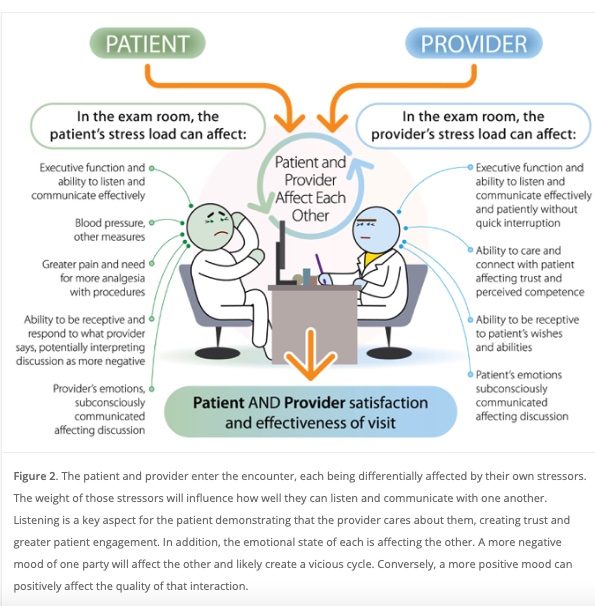
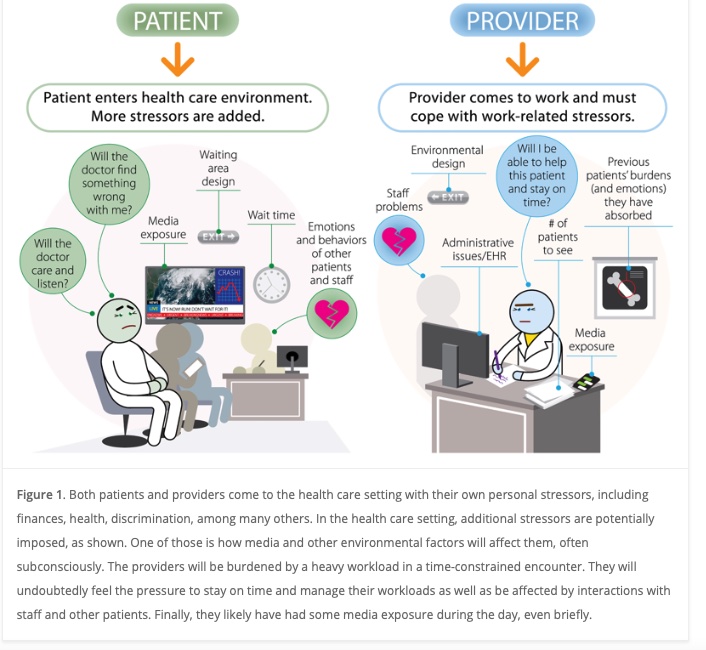
I recently came across an article by Dr David Fryburg on factors including media that affect patient experience in the office setting. The picture below accurately depicts both the patient and provider perspective during the encounter. His study concluded that to ease stress media provided should reflect relaxing music, videos etc. to enhance both the provider’s and patient’s experience in the hospital and clinic setting.
Although he did no talk about appointment times, Id like to talk about gaps in providing the best care for patients who come to us with mental health issues and behavioral challenges. I acknowledge that relaxing clinic and ER waiting area can contribute to better encounters. But the real challenge that we are facing lie in how providers and patients interact, and how the pressure of time can directly affect both provider and patient experience.
Medical issues can be almost accurately evaluated, diagnosed and a treatment plan developed based on diagnostic tests, and patient related information shared by the patient. In mental health, providers are required to provider a diagnosis code so we can bill insurance. What is the diagnosed based on? The diagnosis is based upon the information that the patient is willing to share with you in 30 minutes. Most often details are prompted by the provider’s canned list of questions based on ICD 10 diagnosis criteria and client response to their intake questionnaire (if they decided to fill out the form). Some providers are thoughtful enough to know that one cannot accurately formulate a diagnosis with a 30 minute encounter. Those providers who are prudent , know that it is more appropriate to identify and cite the patient’s specific symptoms instead of designate a permanent label to someone’s crisis based presentation i.e. acute psychosis instead vs schizophrenia.
So what is the point of all of this? Whether we like it or not, everyone suffers from some form of stress, and anxiety on a daily basis. The mental health industry, providers in the field and the demand for their services is sky rocketing. Past trauma, aggravated by the effects of the Pandemic is reflected on reported crimes including, substance use, drug related deaths, violence toward self and others are a reflection of the population’s mental health/wellness as well as the many gaps that separate people from seeking help or getting the help that they need and deserve.
Health (which includes mental health) exist in a continuum. There are good days and there are bad days. However as those bad days become more frequent and become less manageable, there is a potential of getting stuck in a disease state.
We as providers for mental health have a huge responsibility to provide compassionate care for people who come to us for help. We have to remember that care and how effective it is, is not necessarily measured through the number of patients we see, or our reimbursement rates. Mental and behavioral health or illness, crisis present itself when people have maximized their resilience capacity; think of the many years that layers upon layers of self protective mechanisms (that may not be healthy) are developed to survive on a daily basis. Humans are resilient but we have our limits.
As I move forward to create my own self pay practice, it is my hope that providers and HMP’s will see the value in taking the time to allow clients to share their real stories. The PMHNP’s philosophy is based upon on diagnosis and medication management, and a little CBT. However, this should not prevent us from respecting people’s traumas and an understanding that most of the resulting behaviors are considered embarrassing by society. Effective client -provider trusting relationships are impossible to develop in 30 minutes.
Empowered Choices, is a virtual platform that offers mental and behavioral health services, that are driven by both the client and the provider. Accessible, and affordable care, its a choice that we have to make to deliver the right type of care.
Words to Ponder Upon...

Adverse Childhood Events & Trauma
trauma happens more than we dare to admit. Trauma from childhood, often unspoken because we assume we are doing well manifests itself in adulthood without our awareness. As I continue to study about Trauma, it is amazing how many people present at the clinic, misdiagnosed and overly medicated.
Disclaimer
Please note that all materials and information posted on this blog have been generated by Empowered Choices. The opinions expressed in this content are not intended to be taken as official medical advice, but rather the viewpoint of the author. The blog and website content may contain information from other sites, which will be appropriately cited. We cannot guarantee the accuracy, completeness, or reliability of any information presented. We urge you to consult with your personal healthcare professional for any medical concerns or questions you may have. Thank you for your understanding and cooperation.
For any mental health crisis symptoms please call 911 and or go to the nearest Emergency Room.